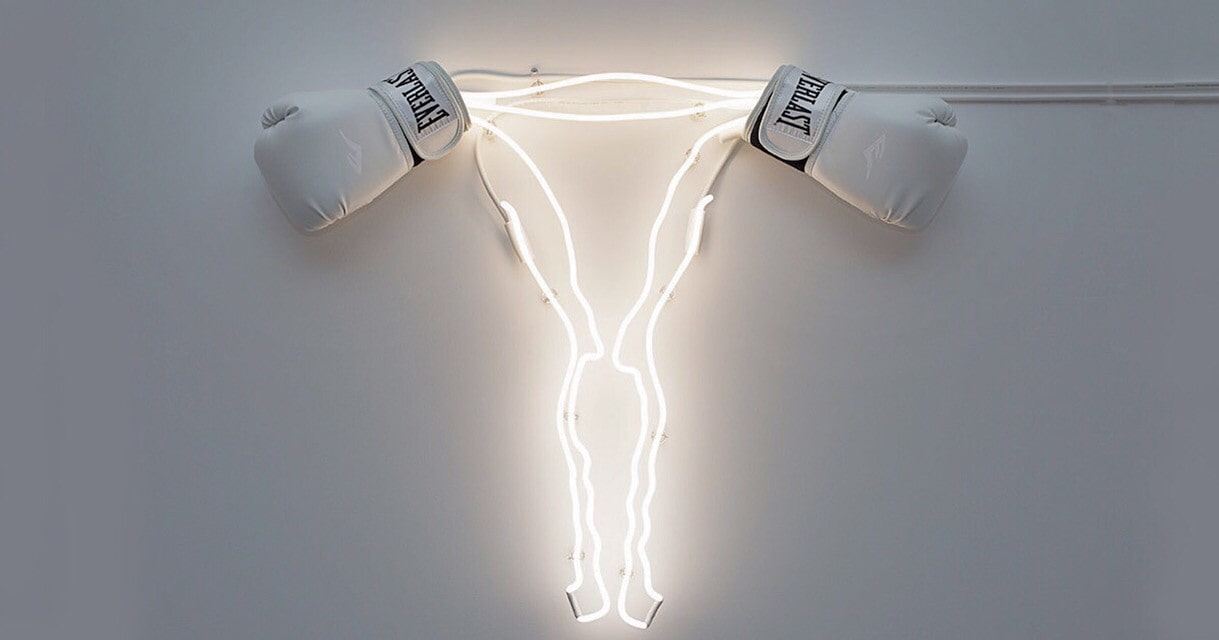
Endometriosis: Here's What You Need To Know (It's Freaking Painful)
For those of us who succumb to the obsessive urge to self-diagnose on the Internet, we know that pain is one of those things that can mean anything from gas all the way to “you’re pregnant and/or dying.” Endometriosis, sometimes colloquially referred to simply as “endo” is a common gynaecological condition that affects reproductive-aged biological women. There are a lot of myths surrounding what endometriosis is exactly, and it is much more than a painful period.
Contrary to popular belief perpetuated by outdated scientific myths, this very complex condition is characterized by the presence of tissue that resembles endometrium (the tissue that lines the uterus and breaks down to be shed during your period), which according to the experts at the Center for Endometriosis Care is an important distinction to make. This endometrial-like tissue generally forms amongst the structures housed in the pelvic region, though it has - however rarely - been found as far from the reproductive system as the brain, and can result in significant chronic pain and inflammation, cysts and lesions, compromised organ, endocrine, and immune systems and more. The permutations of how this condition can manifest are very unique to every affected individual, which only adds to the challenges for diagnosis and treatment.
So Who Is Affected By It?
Endo is not an uncommon affliction. It is estimated that 1 in 10 women have endometriosis, whether they realize it or not. Generally, it’s found in women in their thirties and forties. However, it can affect anyone with a uterus who has reached reproductive maturity, with girls as young as 8 years old having been diagnosed.
How do I get it?
Honest answer: no one really knows.
The cause of endometriosis has yet to be confirmed. But it does seem that it might run in the family. Those with a close family member affected by endometriosis are much more likely to be found to have it as well.
How do I know if I have it?
The most common symptom associated with endometriosis is pain, particularly in the abdominal and pelvic regions. But fear not — even though it might feel like you are, in fact, dying sometimes — it is extremely unlikely that endometriosis will kill you.
Endometriosis symptoms manifest differently from person to person, but the most common include:
- Chronic abdominal, pelvic, and lower back pain
- Severe cramps during menstruation (that may worsen over time)
- Pain during and/or after intercourse
- Pain during ovulation
- Gastrointestinal pain, which can result in nausea, constipation, or diarrhea (which is why endo often gets mistaken for stomach and intestinal conditions such as IBS)
- Painful urination and bowel movements during your period
- Spotting or bleeding between periods
- Infertility

Fun stuff, amirite?
What will really give endometriosis away though is that these symptoms will show up (or significantly worsen) during your period.
Everyone experiences their symptoms differently (with up to 25% experiencing no obvious symptoms whatsoever), which makes it difficult to pinpoint whether or not endometriosis is the cause of your pain. The only way to know for sure is with help of your trusted medical professional.
What happens when I see my doctor?
When your doctor performs a regular pelvic exam, they check by hand for larger cysts or scar tissue that may be hiding around your uterus and ovaries. However, tissue growth typical of endometriosis can be difficult to detect through this technique alone. That’s where medical imaging technology comes into play.
Ultrasounds and MRIs are non-invasive procedures they may perform to take to take fancy pictures of your insides so they can get the inside scoop on what your reproductive organs are up to. If those images do come back with something suspicious, your doctor will likely perform a biopsy on the questionable tissue to confirm your situation.
Give It To Me Straight, Doc: What’s The Worst Case Scenario?
The chronic and extreme pain can affect your daily life in your the ability to work. The financial burden of medical care and treatment can add up. It can severely affect your overall mental well-being and your interpersonal relationships. Not to mention that because of the variety in symptoms, it’s hard to detect, so it can take the average person around 10 years to reach a diagnosis.
Wait, WHAT?!
Also, you might be infertile. And you could need surgery.
Sounds great… Anything else?
Sorry, I should explain. Infertility has been linked to endometriosis as many women will learn that they have endometriosis when they look into why they are having difficulties getting pregnant. But endometriosis does not necessarily cause infertility — many women suffering from endo will go on to have healthy pregnancies, my own mother included.
And surgery is only considered for those with extremely severe symptoms after they’ve tried all the much less invasive measures.
So how do I get rid of it??
You can’t. It’s incurable.
Okay, harsh. How do I live with it then?
There are definitely options when it comes to the treatment and management of endometriosis. Much like the variety in the symptoms themselves, how effective they are will vary from person to person, which means no one treatment can be applied as a healing blanket for everyone.
However, for most, hormonal birth control is a good place to start.

We already know that endo's symptoms can be worsened by menstrual bleeding. Since hormonal birth control can be used to reduce the frequency and intensity of menstrual periods, or stop them all together, they can help reduce (and sometimes even eliminate) the pain that is exacerbated by menstrual bleeding. Hormone-releasing IUDs like Mirena are increasingly in popularity as a treatment for endo for this reason.
However, generally anything that reduces inflammation and bleeding, especially during menstruation, will help reduce the symptoms of endometriosis. Anti-inflammatory and pain medicines like ibuprofen and naproxen, regular exercise, a healthy diet, and reducing caffeine and alcohol consumption can all go a long way to keeping endometriosis in check.
Though it can be a very real and overwhelming challenge to both diagnose and manage, endometriosis is not a death sentence. Through positive and healthy lifestyle choices, raising concerns and exploring options with your doctor, and increasing awareness of this very real and common condition, it is possible for people to live a healthy life in spite of their rebellious uterine tissue.
Cover Photo Source: Zoe Buckman